|
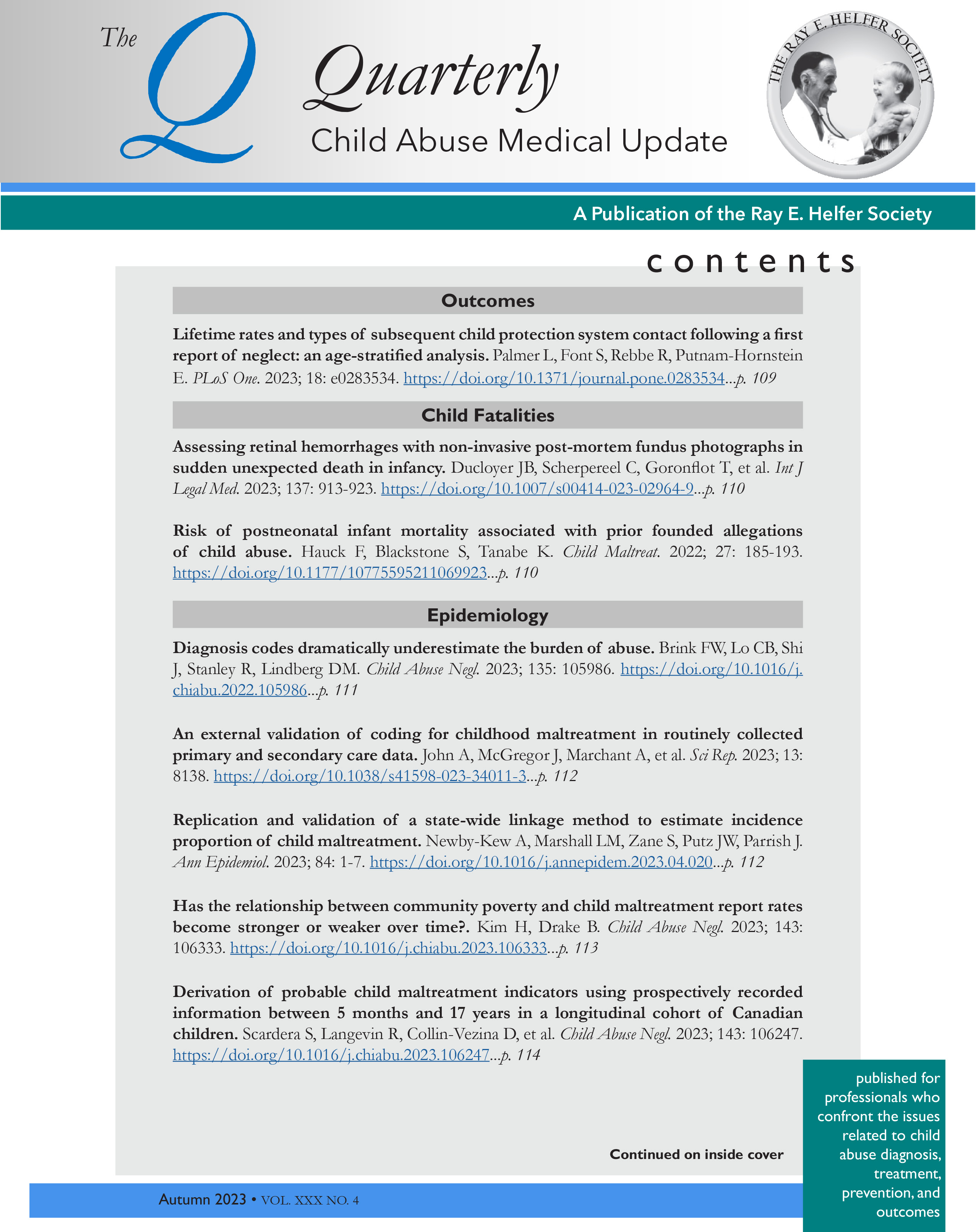
Current Issue Content
Prevention and ResilienceAssociation of maternal risk factors with infant maltreatment: an administrative data cohort study. Smith JN, Guttmann A, Kopp A, et al. Arch Dis Child. 2023; 109: 23-29. https://doi.org/10.1136/archdischild-2022-325239 Hospitalization for physical child abuse: associated medical factors and medical history since birth. Loiseau M, Cottenet J, Francois-Purssel I, et al. Child Abuse Negl. 2023; 146: 106482. https://doi.org/10.1016/j.chiabu.2023.106482 Material hardship in the postpartum year: links to child maltreatment. Marcal K Chang OD, Park Y, Maguire-Jack K. Child Abuse Negl. 2023; 124: 106438. https://doi.org/10.1016/j.chiabu.2023.106438 Early predictors for maltreatment-related injuries in infancy and long-term mortality: a population-based study. Chen HH, Wang IA, Hsieh TW, Tsay JH, Chen CY. BMC Pub Health. 2023; 23: 2232. https://doi.org/10.1186/s12889-023-17180-8 Impact of a parent education program delivered by nurses and health care providers in reducing infant physical abuse hospitalization rates in British Columbia, Canada. Sadler K, Rajabali F, Zheng A, Jain N, Pike I. Can J Nurs Res. 2024; 56: 109-116. https://doi.org/10.1177/08445621231222527 AccidentsPediatric cervical spine injury following blunt trauma in children younger than 3 years: the PEDSPINE II study. Luckhurst CM, Wilberg HM, Brown RL, et al. JAMA Surg. 2023; 158: 1126-1132. https://doi.org/10.1001/jamasurg.2023.4213 Femoral fractures and abuse in children under 36 months old: a Swiss case series. de Marco G, Valaikaite R, Chargui M, et al. J Pediatr Orthop B. 2023; Online ahead of print. https://doi.org/10.1097/BPB.0000000000001140 Emotional AbuseChildhood verbal abuse as a child maltreatment subtype: a systematic review of the current evidence. Dube SR, Li ET, Fiorini G, et al. Child Abuse Negl. 2023; 144: 106394. https://doi.org/10.1016/j.chiabu.2023.106394 EpidemiologyA gap in the data: defining, identifying, and tracking children with medical complexity in the child welfare system. Chung J, Pecora PJ, Sinha A, et al. Child Abuse Negl. 2024; 147: 106600. https://doi.org/10.1016/j.chiabu.2023.106600 Victimization and abuse among children with disabilities: age adjusted rates in a US national sample. Vanderminden J, Finkelhor D, Hamby S, Turner H. Child Abuse Negl. 2023; 146: 106495. https://doi.org/10.1016/j.chiabu.2023.106495 The neighborhood deprivation gradient and child physical abuse and neglect: a Bayesian spatial model. Barboza-Salerno GE. Child Abuse Negl. 2023; 146: 106501. https://doi.org/10.1016/j.chiabu.2023.106501 Imaging and LaboratoryDiagnosis of metaphyseal fractures in infants and young children with suspected inflicted injury: a systematic review of cross-sectional imaging techniques. Alshammari AT, Oates AJ, Rigby AS, Offiah AC. Clin Radiol. 2024; 79: 221-229. https://doi.org/10.1016/j.crad.2023.11.014 Medical Child Abuse – Munchausen Syndrome by ProxyMedical child abuse: medical history and red flags in French adolescents. Abraham-Bizot A, Greco C, Quartier P, et al. Child Abuse Negl. 2023; 146: 106523. https://doi.org/10.1016/j.chiabu.2023.106523 Physical AbuseAssociation between missed appointments and hospitalization for child physical abuse. Callahan R, Johns A, Young A, et al. Heliyon. 2023; 9: e22779. https://doi.org/10.1016/j.heliyon.2023.e22779 Associations between child abuse and neglect, and dento-alveolar injuries in a Children’s hospital population. Azadani EN, McTigue DJ, Peng J, Casamassimo PS. Dent Traumatol. 2023; Online ahead of print. https://doi.org/10.1111/edt.12902 Asymptomatic infant rib fractures are primarily non-abuse-related and should not be used to assess physical child abuse. van Gemert MJC, Vlaming M, Gabaeff SC, Nikkels PGJ, Martino Neumann HA. Children (Basel). 2023; 10: 1827. https://doi.org/10.3390/children10111827 Data-driven evidence shows truthful caregiver histories and significant overdiagnosis of abusive head trauma. Brook CB. Ann Child Neurol Soc. 2023; 1: 299-304. https://doi.org/10.1002/cns3.20035 Disguised incorporation bias and meta-analysis of diagnostic accuracy studies. Lynoe N, Erksson A. Acta Paediatr. 2024; 113: 503-505. https://doi.org/10.1111/apa.17076 Defining sentinel injuries of suspected child abuse by age using international classification of diseases-10: a delphi study. Kim HB, Noh H. Pediatr Emerg Care. 2023; 39: 918-922. https://doi.org/10.1097/PEC.0000000000003029 Multiorgan dysfunction syndrome in abusive and accidental pediatric traumatic brain injury. McNamara CR, Even KM, Kalinowshi A, et al. Neurocrit Care. 2023; Online ahead of print. https://doi.org/10.1007/s12028-023-01887-y Subdural hematoma, retinal hemorrhage, and fracture triad as a clinical predictor for the diagnosis of child abuse. Mamaril-Davis JC, Riordan K, Sumdani H, et al. J Neurosurg Pediatr. 2023; 33: 142-148. https://doi.org/10.3171/2023.11.PEDS23212 Professional and Systems IssuesHow medical students’ trauma histories affect their clinical clerkship experiences. Neff K, McKean E, Miller M, et al. Clin Teach. 2024; e13734. https://doi.org/10.111/tct.13734 Medical professional reports and child welfare system infant investigations: an analysis of National Child Abuse and Neglect Data System data. Edwards F, Roberts SCM, Kenny KS, et al. Health Equity. 2023; 7: 653-662. https://doi.org/10.1089/heq.2023.0136 Initial development of tools to identify child abuse and neglect in pediatric primary care. Hanson RF, Zhu V, Are F, et al. BMC Med Inform Decis Mak. 2023; 23: 266. https://doi.org/10.1186/s12911-023-02361-7 Traumatic stress symptoms and PTSD risk in children served by Children’s Advocacy Centers. McGuier EA, Campbell KA, Byrne KA, Shepard LD, Keeshin B. Front Psychiatry. 2023; 14: 1202085. https://doi.org/10.3389/fpsyt.2023.1202085 SCAN for abuse: electronic health record-based universal child abuse screening. Martin N, Claypool AL, Diyaolu D, et al. J Pediatr Surg. 2024; 59: 337-341. https://doi.org/10.1016/j.jpedsurg.2023.10.025 Public PolicyImpact of a family treatment court on child permanency and safety. Mersky JP, Lee CP, Janczewski CE. Child Abuse Negl. 2023; 146: 106512. https://doi.org/10.1016/j.chiabu.2023.106512 State policies on child maltreatment and racial disproportionality. LaBrenz CA, Littleto T, Shipe S, Bai R, Stargel L. Child Youth Serv Rev. 2023; 151: 107048. https://doi.org/10.1016/j.childyouth.2023.107048 Public benefit programs and differential associations with child maltreatment by race and ethnicity. Puls HT, Hall M, Boyd R, Chung PJ. JAMA Pediatr. 2024; 178: 185-192. https://doi.org/10.1001/jamapediatrics.2023.5521 Related Disease StatesCerebral sinovenous thrombosis as a cause of subdural hemorrhage in the pediatric population: is there a correlation?. Serra SMB, de Oliveira RRB, Galvao IFG, Maia JS. Childs Nerv Syst. 2024; 40: 603-605. https://doi.org/10.1007/s00381-023-06199-2 The role of intrapartum fetal head compression in neonatal retinal hemorrhage. Lam MR, Yang CD, Comenarez JA, et al. JAAPOS. 2023; 27: 267.e1-267.e7. https://doi.org/10.1016/j.jaapos.2023.07.013 Sexual AbuseChild sexual abuse: comparison of male and female victims. Lupariello F, Lauria b, Mirri F, et al. Am J Forensic Med Pathol. 2024; 45: 33-39. https://doi.org/10.1097/PAF.0000000000000902 A systematic review of factors associated with disclosure of child sexual abuse. Abdul Latiff M, Fang L, Goh DA, Tan LJ. Child Abuse Negl. 2023; 147: 106564. https://doi.org/10.1016/j.chiabu.2023.106564 Female adolescent sexual assault; a national review of 1014 consecutive cases. Kane D, Eogan M. J Forensic Leg Med. 2023; 101: 102613. https://doi.org/10.1016/j.jflm.2023.102613 Barriers to seeking medical care among youth victims of sexual violence. Kamke K, Mullin TM, Goodman KL. J Adolesc Health. 2023; 73: 1077-1082. https://doi.org/10.1016/j.jadohealth.2023.06.034 Integrating social care into a specialized medical home for sex-trafficked youth. Raj A, Krass P, Hackett K, Green S, Wood JN. Pediatrics. 2024; 153: e2023062394. https://doi.org/10.1542/peds.2023-062394 Gonorrheal and chlamydia yield for genital and extragenital testing in children evaluated for sexual abuse. Nasrazadani A, Ruda M, Girardet R, et al. Child Abuse Negl. 2024; 147: 106525. https://doi.org/10.1016/j.chiabu.2023.106525 Anogenital injury following sexual assault and consensual sexual intercourse: a systematic review and meta-analysis. Naumann DN, Morris L, Bowley DM, et al. EclinicalMedicine. 2023; 65: 102266. https://doi.org/10.1016/j.eclinm.2023.102266 |


 Spring
Spring